Blogs
- Home
- Blogs
- Educational
- What is PGT-A & Who Should Consider It?

What is PGT-A & Who Should Consider It?
October 14, 2024Molly Chu Chen - Labryo Fertility
EducationalAssisted reproductive technology (ART), such as in vitro fertilization (IVF), has helped many individuals and families lighten the burden of infertility. However, even with IVF, the risk of miscarriages or the birth of a child with genetic abnormalities remains. Thus, genetic testing can be crucial in increasing the chances of a successful pregnancy with a healthy baby.
One of the most common types of preimplantation genetic testing (PGT) used during IVF treatment is PGT-A testing. This article will delve into the details of this genetic screening procedure, explaining what PGT-A tests for, who should consider it, the steps involved, and the potential benefits, helping patients make informed decisions during their fertility treatment.
1. What is PGT-A Testing?
Preimplantation genetic testing for aneuploidy (PGT-A) was previously known as preimplantation genetic screening (PGS). It is a screening procedure that evaluates the number of chromosomes in embryos within the limits of test resolution.
1.1 What Does PGT-A Test For?
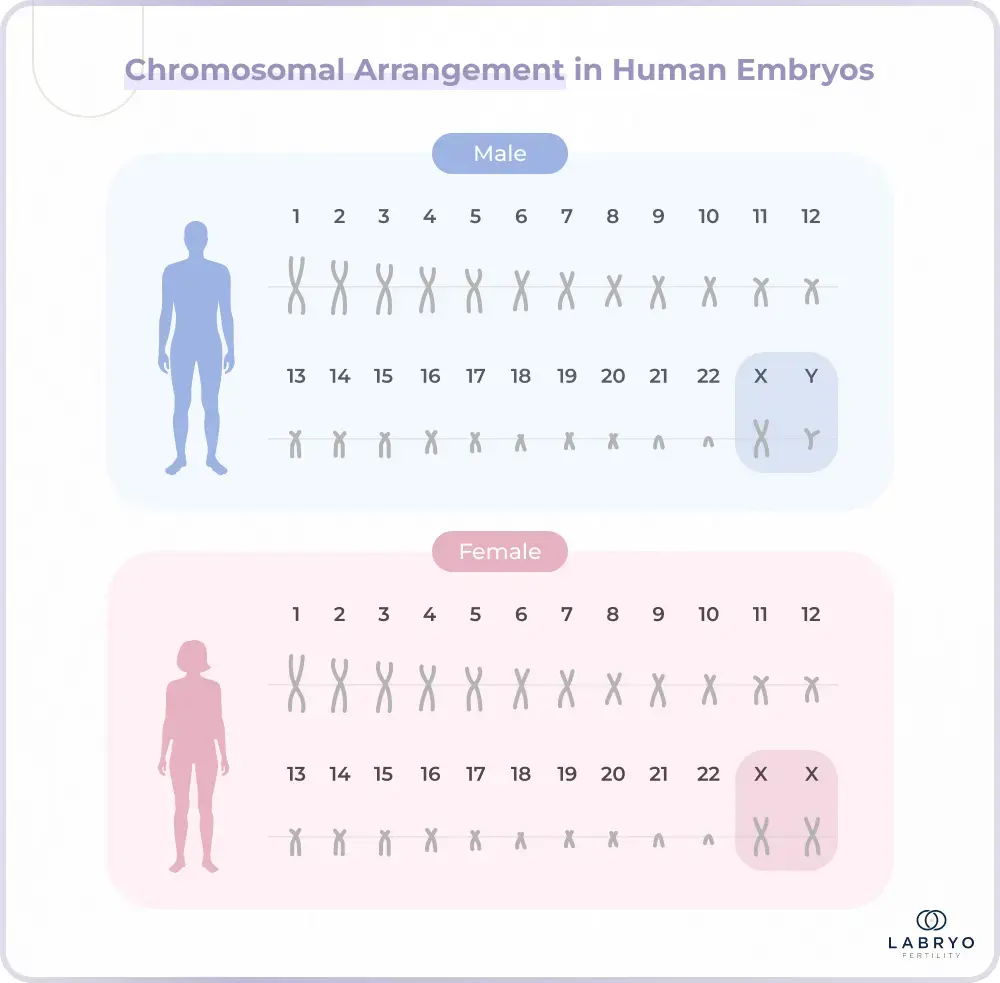
Chromosomes are the structures that contain genetic material within our cells. A healthy human embryo should have 46 chromosomes arranged in 23 pairs, including 22 pairs of autosomes (numbered chromosomes) and 1 pair of sex chromosomes (XX for females, XY for males). Also, 23 pairs of these chromosomes come from the egg, while the other 23 pairs come from the sperm.
PGT-A tests embryos to determine whether they are euploid (normal) or aneuploid (abnormal). Euploid embryos have a full set of 46 chromosomes. Aneuploid embryos, on the other hand, have missing or extra chromosomes. Additionally, aneuploidy can be further classified into:
- Trisomy: This condition involves an extra copy of a chromosome. In the most common example, Down syndrome (trisomy 21), individuals have three copies of chromosome 21, resulting in a total of 47 chromosomes.
- Monosomy: This condition involves a missing chromosome. For instance, Turner syndrome, a form of monosomy, occurs when a female has only one X chromosome instead of two, resulting in a total of 45 chromosomes.
- Triploidy: This condition involves an entire extra set of chromosomes, having 69 chromosomes instead of 46 (each set has 23 chromosomes), which is incompatible with life.
1.2. Why is It Important to Test for Aneuploidy?
According to research by the American Society of Human Genetics, aneuploid embryos have up to 86.3% risk of miscarriage as they usually experience difficulty implanting in the uterus. Even if the embryos are implanted successfully, aneuploid embryos may still have difficulty in developing.
Consequently, this can lead to genetic disorders (e.g. Down syndrome, Turner syndrome, and Klinefelter syndrome) within the future child. By screening the embryos through PGT-A, intended parents can exclude aneuploid embryos for transfer cycles in IVF, minimizing the risks of these issues.
1.3 Who Should Consider PGT-A?
PGT-A testing is available for most females undergoing IVF and it is often recommended for patients who:
- Are over 35 years old
- Have a history of multiple miscarriages (two times or more)
- Experienced multiple failed IVF treatments
- Previously had a child with aneuploidy or other genetic conditions
- Have a family history of chromosomal issues
This is because chromosomal abnormalities occur by accident during the formation of eggs or sperm (meiosis) or in the early stages of fetal development (mitosis), and research by the National Human Genome Research Institute suggests that the maternal age and environmental factors could potentially increase the risk of such conditions. Hence, patients should consult their fertility specialist to decide whether or not they should use PGT-A based on their personal circumstances.
2. How Does PGT-A Testing Improve IVF Success Rates?
A study in Reproductive Biomedicine shows that PGT-A-tested embryo transfers resulted in higher live birth rates than non-PGT-A transfers, both for fresh (49.5% vs. 38.6%) and frozen embryos (50.6% vs. 35.8%). This contrast is particularly prevalent when patients have a higher maternal age, as seen in the graph below:
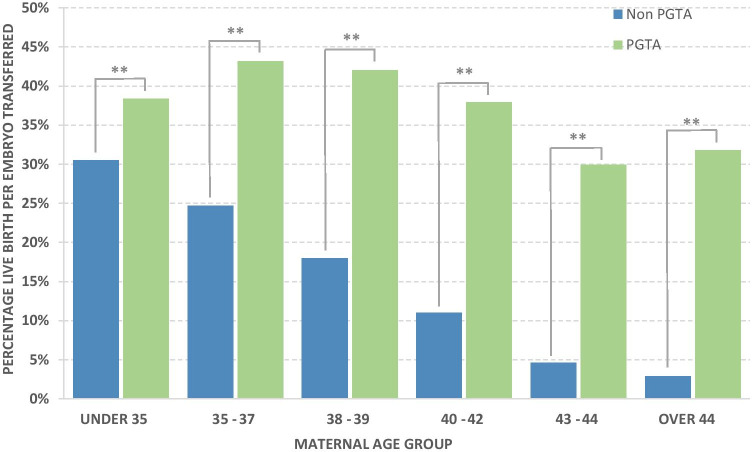
Although PGT-A does not directly alter an embryo's chromosomes or screen for specific genetic conditions, it can help choose the most viable embryo for transfer during infertility treatments. Not only can this minimize the risk of miscarriages and congenital conditions at birth, but it can also reduce the risk of multiple gestational pregnancies per IVF cycle, thus increasing the likelihood of a safe and healthy pregnancy.
3. What is the Difference between PGT-A, PGT-SR, and PGT-M?
These three procedures assess embryos for different genetic conditions. Unlike PGT-A, PGT-SR (preimplantation genetic testing for structural rearrangements) tests for structural abnormalities in chromosomes, such as translocations or inversions, which can increase the risk of chromosomal imbalances in embryos. On the other hand, PGT-M (preimplantation genetic testing for monogenic disorders) tests for specific single-gene disorders, such as cystic fibrosis or sickle cell anemia.
| Test Type | PGT-A | PGT-SR | PGT-M |
|---|---|---|---|
| Screening Factor | Extra or missing number of chromosomes | Chromosomal rearrangements | Specific single-gene conditions |
| Purpose | Prevent miscarriages or congenital issues related to aneuploidy | Prevent miscarriages related to translocations or inversions | Prevent X-linked, autosomal recessive, and autosomal dominant diseases |
| Recommended For | All IVF patients, especially women in a higher age group | Patients who are carriers of chromosomal imbalance | Patients with a history of genetic disorders or those who are recessive carriers |
4. The PGT-A Testing Process: 6 Key Steps Explained
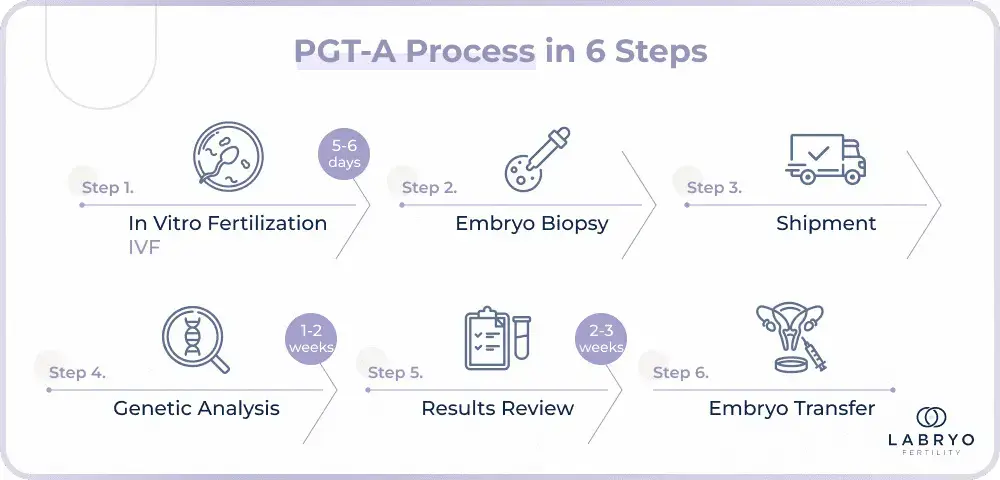
So, how does PGT-A work? If you're considering PGT-A, it's essential to discuss your options with your fertility specialist early on. The entire process could take 2 to 6 weeks so it must be planned ahead to be integrated into the IVF treatment plan. Here are the steps involved:
Step 1. In Vitro Fertilization (IVF)
Patients will undergo hormone stimulation with medication to produce multiple eggs. These eggs are then retrieved and fertilized with sperm to create an embryo within the clinic’s laboratory.
Step 2. Embryo Biopsy
Once the embryos reach the blastocyst stage after 5 to 6 days, a few cells will be collected as samples. At this stage, each embryo consists of 50-150 cells, some of which will develop into the fetus and others into the placenta. Only cells from the outer layer, the ones that will become the placenta, will be biopsied for PGT-A testing as this minimizes the risk of harming the embryo.
Step 3. Shipment
The embryos will then be frozen immediately after biopsy and stored at the fertility clinic, while the biopsied cell samples are sent to a specialized genetic laboratory for analysis.
Step 4. Genetic Analysis
With advanced equipment, the genetic laboratory will examine all the embryos' chromosomes to determine if there are any abnormalities.
Step 5. Results Review
After 1 to 2 weeks, the PGT-A results will be sent back and reviewed by the patient’s fertility specialist. The patient will receive a detailed report that outlines the chromosomal status of each embryo, classifying them into four possible result types:
- Euploid (Normal): These embryos have 23 pairs of chromosomes (46 in total), which is the correct number for healthy development. They are ideal for implantation as they have the highest chance of resulting in a successful pregnancy.
- Aneuploid (Abnormal): These embryos have chromosomal abnormalities, such as missing or extra chromosomes, or irregular shapes. They are typically not recommended for transfer.
- Mosaic (Mixed): These embryos contain a mix of normal and abnormal cells. The viability of mosaic embryos depends on the ratio of healthy to abnormal cells. Some lower-risk mosaic embryos may still be considered for transfer if they have a high probability of leading to a healthy pregnancy.
- No Result (Inconclusive): In some cases, the test fails to produce a clear result due to insufficient DNA or poor sample quality. If this happens, the fertility specialist may recommend re-testing or considering other options.
Step 6. Embryo Transfer
Using the PGT-A results, IVF patients can select the suitable embryo(s) for transfer. The doctor will prescribe medication to thicken the patient’s uterine lining and transfer the thawed embryo after 2 to 3 weeks.
5. Frequently Asked Questions About PGT-A Testing
5.1 Does PGT-A have any risks?
PGT-A itself does not pose additional risks to the IVF patient. Nonetheless, there are potential risks associated with the biopsy and testing that may affect the embryos:
- Inaccurate Results: While PGT-A is highly accurate, as with any test, there is a chance for errors. Examples include but are not limited to false positives indicating an abnormality that isn't present or false negatives that miss an existing abnormality.
- Potential Damage to the Embryo: The biopsy process involved in PGT-A can carry a small risk of damaging the embryo and stunting its development, but this can be prevented by choosing an IVF lab with experienced and skilled embryologists.
- Embryo Discards: If the embryos tested are aneuploid, they may be discarded, This reduces the amount of embryo available for transfer. In the instance that all embryos are discarded, patients will have to go through another retrieval cycle.
If an IVF patient isn’t sure about the potential risks of PGT-A, it is recommended to discuss it with their fertility specialist. The doctors will provide personalized guidance based on each patient’s individual circumstances.
5.2 How much does PGT-A cost? Is it covered by insurance?
The average cost of PGT-A ranges from $4,000 to $10,000. This is influenced by several factors, including the number of embryos tested, the location of the fertility clinic, insurance coverage, etc.
Some insurance plans may partially or fully cover PGT-A, while others may not, so patients will have to check with their insurance provider to determine the specific coverage. Even if the insurance doesn't cover PGT-A, several fertility clinics offer financing options to make the procedure more affordable.
5.3 Can PGT-A be done if the sperm or eggs are from anonymous donors?
Typically, PGT-A can be performed without additional DNA samples from the sperm or egg donor. The genetic analysis is based on the DNA extracted from the embryos themselves. However, for PGT-M, additional DNA samples may be required so it's best to consult with a fertility specialist to determine the specific requirements.
5.4 Can PGT-A be used to screen gender?
Yes, PGT-A can be used for gender selection. While its primary purpose is to screen for chromosomal abnormalities, the same process can also identify the embryo’s sex. This information can be used to avoid gender-linked genetic disorders. But, it's crucial to note that gender selection using PGT-A may not be readily available in all regions. It is also important for you to know that PGT-A testing can be done where gender is masked if one does not want to know the gender beforehand.
5.5 What does it mean when a PGT-A shows “no result”?
A "no result" in PGT-A signifies that the test could not determine the chromosomal status of the embryo. This outcome may stem from two reasons:
- Embryo Quality or Chromosome Quantity Issues: Embryos with poor-quality chromosomes or an insufficient number of chromosomes may not develop properly to the blastocyst stage (days 5–6 post-fertilization), making them unsuitable for biopsy. In such cases, the reproductive endocrinologist might recommend repeating ovarian stimulation to retrieve new eggs, aiming for embryos with better chromosomal quality for the next PGT-A.
- Incorrect Interpretation: PGT-A only takes a sample of 5-6 cells from the outer layer of the embryo, which will form the placenta. This sample may not always reflect the entire embryo's chromosomal makeup, especially in mosaic embryos, which have a mix of normal and abnormal cells. If the biopsy sample contains only abnormal cells, even if the embryo is mostly normal, it can lead to an inconclusive result. So, a repeat biopsy may be ordered to clarify the result.
Nevertheless, when a "no result" occurs, it’s important to consult with your fertility specialist to determine the most appropriate course of action based on individual circumstances.
6. Why Choose Labryo Fertility Center for PGT-A Testing?
An experienced IVF clinic will work with a PGT-A testing laboratory to provide accurate screening results, which can help increase the chances of a healthy pregnancy.
Labryo Fertility Center is a trusted destination for PGT-A testing and IVF treatments. Leveraging the latest advancements in reproductive medicine, our expert team is committed to providing top-tier personalized care throughout your fertility journey.
We offer a wide range of fertility services, including IVF, PGT-A, and other diagnostic procedures, helping you receive all the necessary support in one convenient location. Contact Labryo Fertility Center and schedule a consultation with us today.
Read More:
- Gestational Surrogacy Success Rates
- How Much Does IVF Cost in California?
- Egg Freezing/Oocyte Cryopreservation Cost & Financing Plans
Meet Our Experts Guiding You Through PGT-A
In hopes of making sure all patients are well-informed in their journey to parenthood, this article on PGT-A is brought to you by Labryo Fertility Center’s experts, Molly Chu-Chen, and Dr. Jeremy A. King.
Molly Chu-Chen, M.S., M.H.A., TS (ABB) - Chief Embryologist & Founder

Molly Chu-Chen has over two decades of expertise in embryo evaluation and genetics. Certified as a Technical Supervisor by the American Board of Bioanalysis, Molly has played a key role in advancing preimplantation genetic testing, including PGT-A, to improve embryo selection and pregnancy outcomes. Her training in top institutions across the U.S., Taiwan, and Singapore empowers her to combine global best practices with cutting-edge lab techniques. She also remains closely involved in every case, ensuring each embryo is treated with the care it deserves.
Dr. Jeremy A. King, M.D. - Director of IVF

Dr. Jeremy A. King brings groundbreaking expertise to the field of reproductive genetics. With a fellowship in Reproductive Endocrinology and Infertility from Johns Hopkins, Dr. King has published extensively on congenital disorders and hormonal function. His leadership in offering comprehensive PGT-A screening ensures patients receive scientifically sound guidance tailored to their unique genetic profile. Recognized for his patient-first approach, Dr. King also works closely with Labryo Fertility Center’s embryologists to maximize the success of genetically healthy embryo transfers.
