Services
IVF
IVF
What is in vitro fertilization (IVF)?
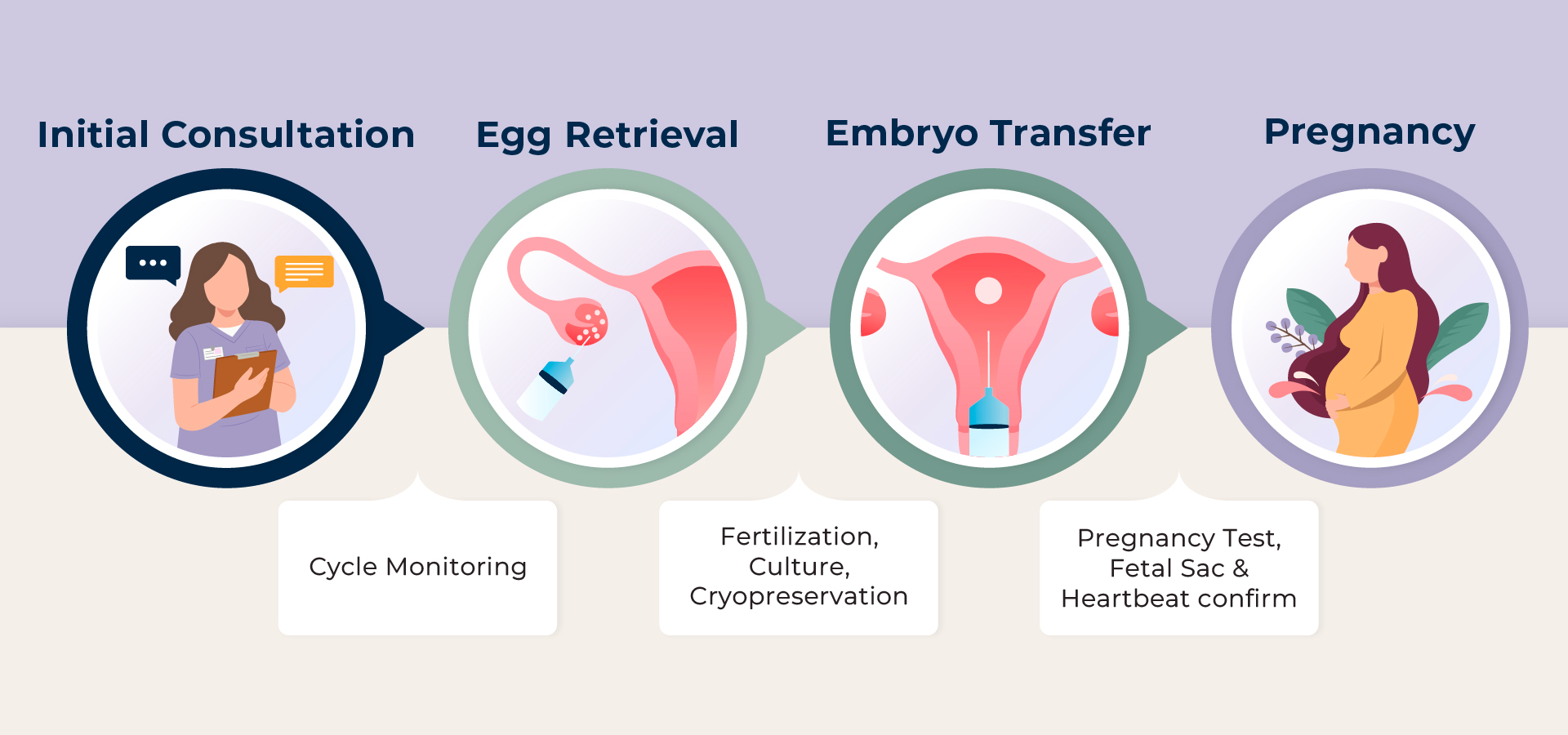
IVF is a method of assisted reproductive technology (ART) in which the sperm and egg are combined outside of the patient’s uterus in a laboratory dish. One or more fertilized eggs (embryos) are then transferred into the woman’s uterus, where the embryo can implant in the uterine lining and begin to develop. Patients can also concurrently cryopreserve (freeze) their extra embryos for future use.

A. Before You Start
1. Initial Consultation
Our physician will review your medical history and discuss which treatment options are for you. For out-of-state or international patients, we also offer an initial video consultation.
2. Financial Consultation
We will explain our different treatment packages and prices, review the fees, discuss various options for you, and provide a quote for recommended treatment.
3. Consent
It is very important for patients and their partners to read through the consent forms and initial/sign as needed.
4. Infectious Disease Panel
To be compliant with the regulations of the state law, we are required to conduct infectious disease testing for both you and your partner before every IVF treatment.
5. Pre-IVF Bloodwork
Our physicians may require you to do bloodwork and exams to further evaluate your health and well-being before you begin treatment, such as testing your TSH, Blood Typing, and Pap Smear.
6. Ovarian Reserve Testing
This test must be done on cycle Day 2 or 3 of your menstrual cycle to evaluate ovarian function.
7. Genetic Testing
The following genetic carrier testing is recommended by the American Society for Reproductive Medicine.
8. Pelvic Ultrasound & Saline Infusion Sonogram (SIS) Testing
All patients need a pelvic ultrasound and a SIS test to evaluate the status of the ovaries, tubes, and uterus.
B. Treatment Schedule
This is usually the treatment cycle of IVF. Now, there are different ways Labryo can approach the egg retrieval part and the embryo transfer part of IVF, depending on your needs and priority.
Different Approaches to the Egg Retrieval Cycle
1. Stress-Free IVF
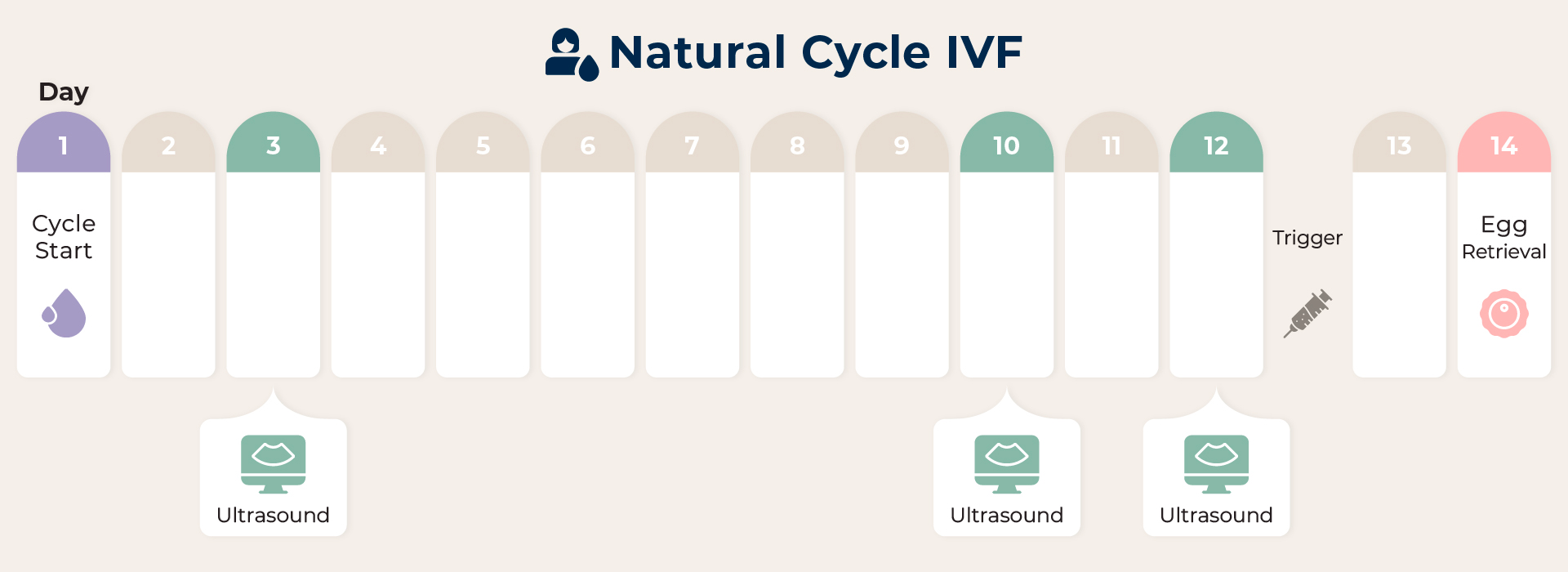
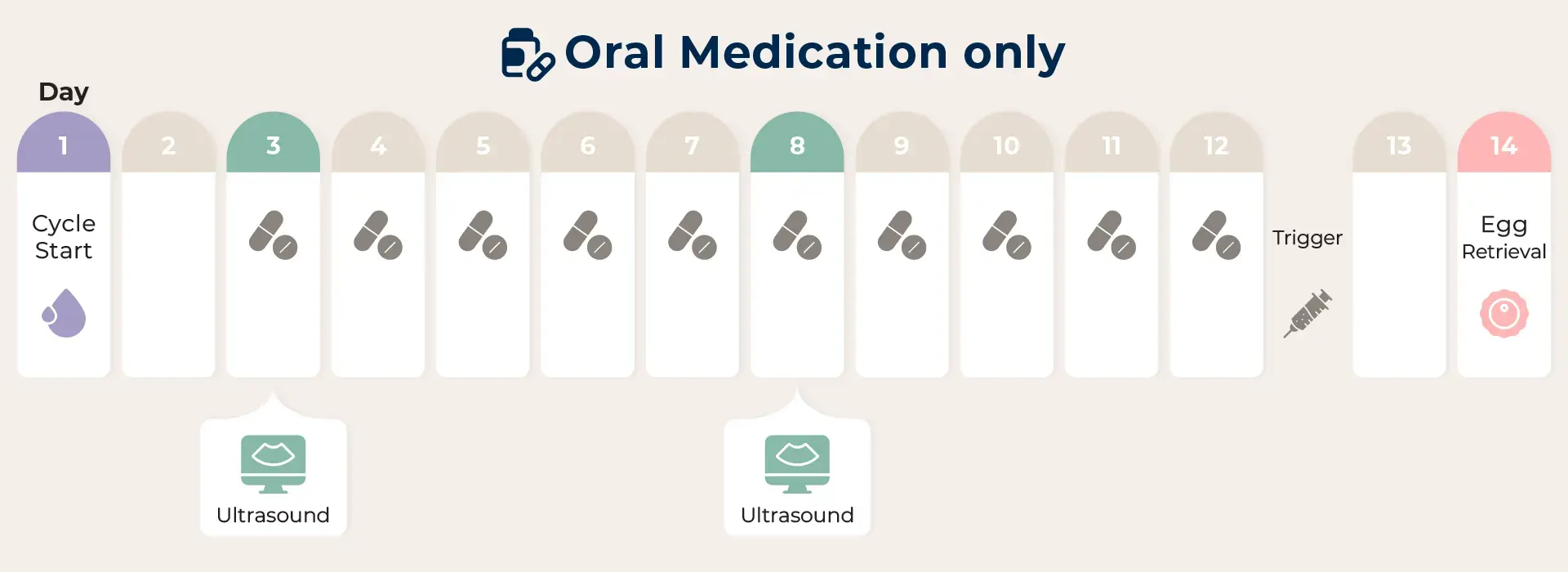
This method is most effective on younger patients or those with a normal menstrual cycle and no problems with ovarian function. With no hormone stimulation or only the use of oral medication to induce follicle maturation, patients have a higher chance of obtaining higher-quality eggs with a low drug impact but will expect to obtain between 1 and 3 eggs per cycle.
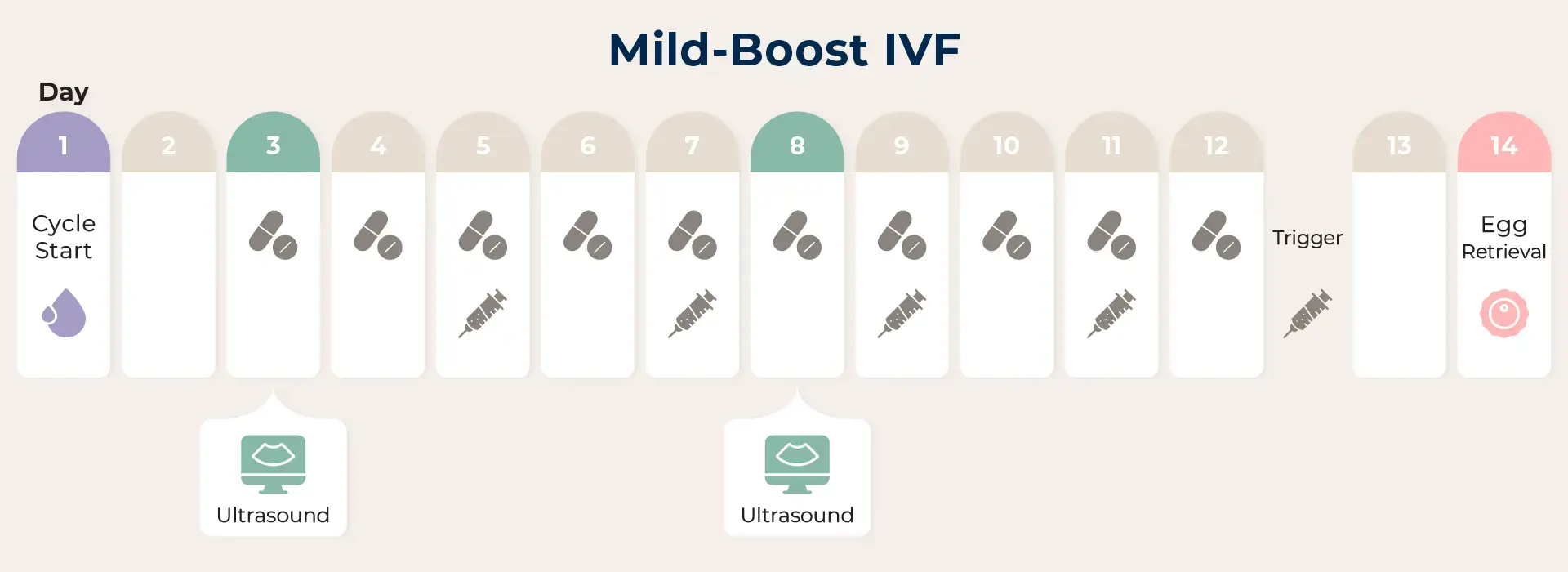
2. Mild-Boost IVF
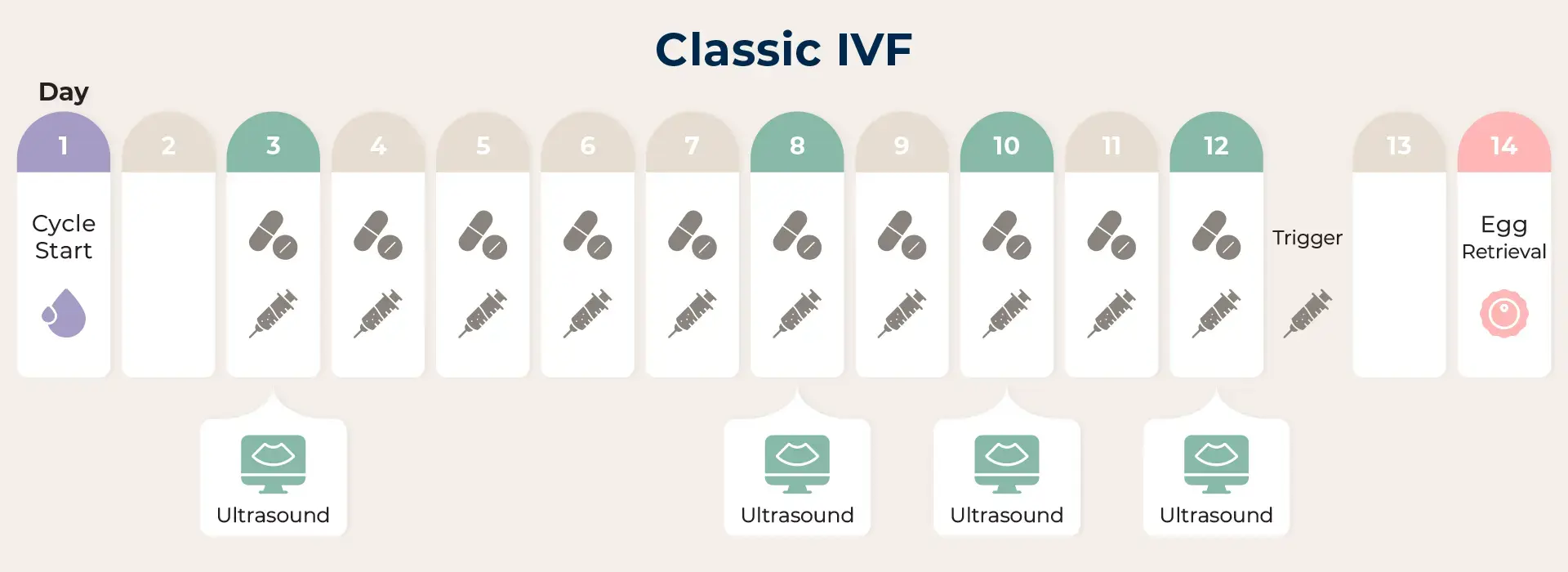
3. Classic IVF
Embryo Transfer Cycle
1. Embryo Transfer
The next step in the IVF process is the embryo transfer. This step requires no anesthesia, though some patients may wish to have a mild sedative. This procedure is usually painless, though some women experience mild cramping.
2. Pregnancy Screening
After the embryo transfer, the first pregnancy blood test will be 10-12 days after the transfer date. After 8-10 weeks of gestation, patients are finished with our clinic’s services and will be referred to a local OBGYN.
