Services
IUI
IUI
What is Intrauterine Insemination (IUI) ?
Intrauterine insemination (IUI), also known as artificial insemination, is a procedure that bypasses the cervix and directly places the sperm in a woman’s uterus around the time of ovulation, and it is performed around the time of ovulation.
By placing the sperm directly into the uterus, this procedure gives the sperm a better chance at making their way to the egg. This process takes less than two hours to complete.
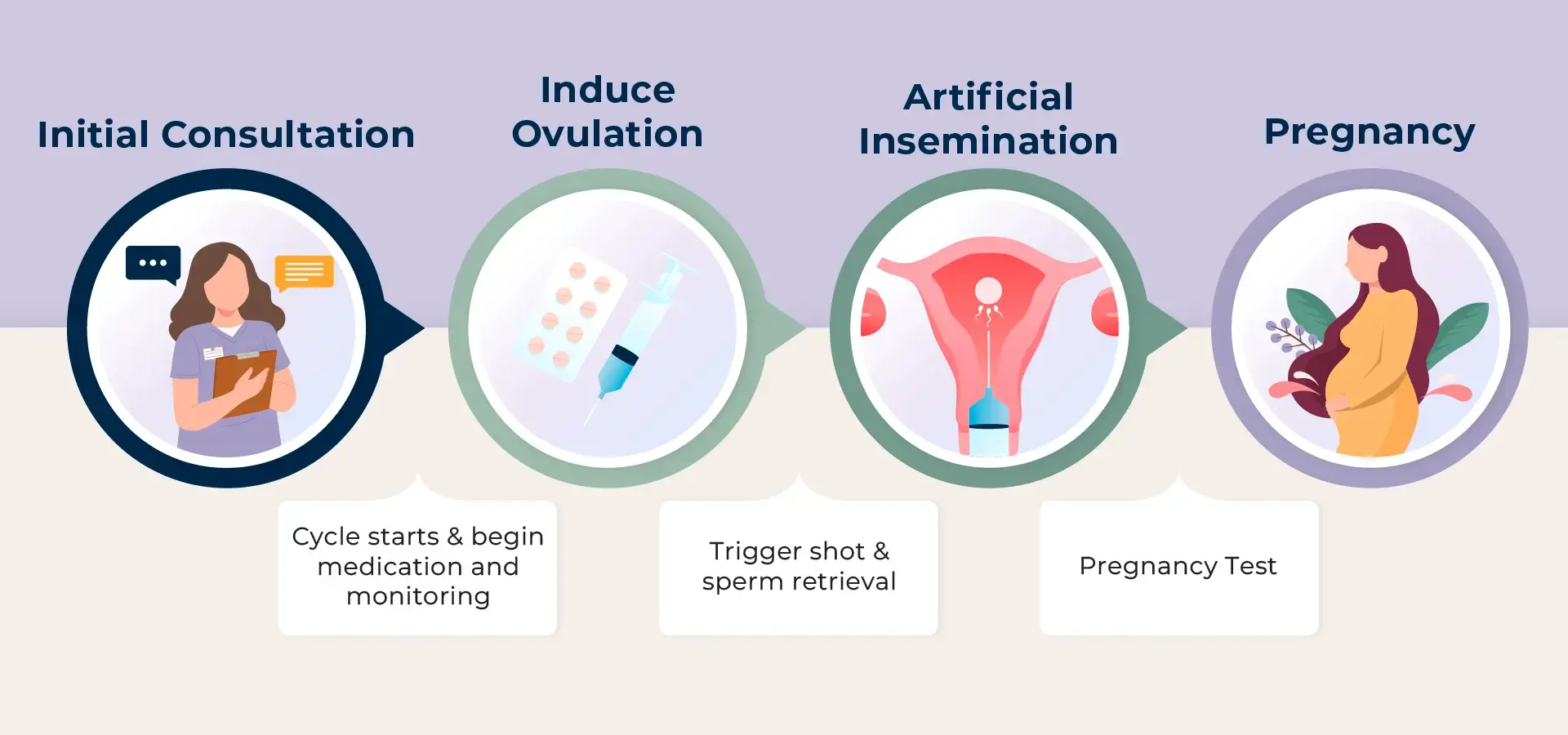
Intrauterine Insemination Process Timeline

