Our IVF Lab
- Home
- Our IVF Lab
- flow
Our IVF Lab
Browse Topics
Our IVF Lab
An IVF laboratory plays a critical role in assisted reproductive technology (ART), ensuring that sperm and eggs are carefully handled to create the healthiest possible embryos for a successful pregnancy in IVF treatments.












At Labryo Fertility Center, we are committed to delivering exceptional lab practices and personalized fertility care. Our state-of-the-art IVF lab is CAP-accredited and CLIA-certified, meeting the highest industry standards. Additionally, our surgery center is Quad A-accredited, ensuring a safe and regulated setting for fertility procedures. With a team of highly skilled embryologists and cutting-edge reproductive technologies, Labryo Fertility Center provides a tailored approach to help each patient achieve their dream of parenthood.
What Happens in an IVF Lab?
The majority of the IVF treatment process will unfold in the IVF lab once the patient has done their part in self-administering fertility medications and going through egg retrieval. Within this specialized environment, our highly trained embryologists meticulously monitor every stage with advanced technologies to ensure the best possible outcomes in these IVF lab procedures:
Egg and Sperm Preparation
Before fertilization can take place, both the eggs and sperm must be carefully prepared in the IVF lab to optimize their quality and viability.
For egg preparation, follicular fluid containing the eggs is handed over to an embryologist after a fresh egg retrieval. Using a high-powered microscope, the eggs are identified and isolated before being rinsed in a specialized culture medium and placed in incubators that mimic conditions inside the human body.
Around two hours after retrieval, the incubated eggs are examined for maturity. Only mature (MII) eggs are selected for fertilization, while immature eggs may be cultured for further development or discarded if non-viable.
In the case of using frozen eggs, the embryologists will thaw the eggs before identifying each one and selecting the eggs suitable for further culture or fertilization.
On the other hand, a semen sample is typically collected on the day of egg retrieval, either through natural ejaculation or, in special cases, via surgical sperm extraction methods like TESA (Testicular Sperm Aspiration) or TESE (Testicular Sperm Extraction).
The semen sample is first assessed for motility, concentration, and morphology before undergoing purification. This is done using density gradient centrifugation (where the sperm are spun at high speed and forced to move through culture mediums with different densities) or the swim-up method (where the sperm is left to naturally swim to the top of the tube) to separate the most highly motile and structurally normal sperm.
If a frozen sperm sample is used, it is thawed and processed in the same manner. Once these procedures are complete, the prepared sperm are then stored in an incubator until fertilization.

Source: Freepik
ICSI & PICSI
Intra-Cytoplasmic Sperm Injection (ICSI) and Physiological ICSI (PICSI) are advanced fertilization techniques that represent some of the greatest ART technology breakthroughs in the past 20 years.
Unlike conventional IVF, where sperm and eggs are combined in a dish to allow natural fertilization, ICSI involves the direct injection of a single, carefully selected sperm into a mature egg using a microscopic needle, while the egg is stabilized under the microscope with a special micro-holding pipette.
PICSI is an advanced version of ICSI. It involves an additional selection process where the embryologist will identify the sperm that binds to hyaluronic acid, a substance naturally found in the egg’s outer layer, before injecting it into the egg.
While we still offer the option of natural fertilization, we would recommend ICSI and PICSI to most of the intended parents as it is particularly beneficial for patients with male factor infertility (such as low sperm count, poor motility, or abnormal morphology), previous fertilization failure in standard IVF, or cases with anti-sperm antibodies affecting fertilization.
The ICSI or PICSI is performed on the day of egg retrieval (Day 0), in the afternoon. After injection, the fertilized eggs are incubated, and embryologists evaluate fertilization after 18 to 22 hours (Day 1). Patients will then be informed of their fertilization results via phone call or email on the afternoon of Day 1.
Source: Freepik
Blastocyst Culture
Blastocyst culture is a process that allows embryos to develop for three to seven days before freezing them in preparation for the patient’s embryo transfer cycle. As the embryos reach the blastocyst phase during culture, the chances of successful implantation increase, so we strongly suggest culturing all embryos to full blastocysts before transferring them.
However, it is important to understand that not all embryos make it to this stage. Thus, our experienced embryologists and physicians will consider the unique circumstances of each patient to give personalized recommendations, ensuring that all the patient’s decisions are well-informed and based on their best interests.

Source: Freepik
Preimplantation Genetic Testing
Preimplantation Genetic Testing (PGT) is an advanced screening process used to evaluate embryos for genetic abnormalities or determine the gender before transfer in IVF treatments. This technique involves carefully removing 3 to 4 cells from a blastocyst-stage embryo to assess its chromosomal integrity and genetic health, doing no harm to the embryos while ensuring only the healthiest embryos are selected for implantation.
At Labryo Fertility Center’s laboratory, we offer the following PGT options:
- PGT-A (Aneuploidy Screening): Identifies embryos with the correct number of chromosomes. Can also provide the gender if intended parents would like.
- PGT-M (Monogenic Disorder Screening): Detects inherited genetic diseases such as cystic fibrosis or sickle cell anemia.
- PGT-SR (Structural Rearrangement Screening): Examines embryos for chromosomal translocations or deletions.
PGT is an optional procedure, and our fertility specialists will discuss with you whether it could be beneficial for your specific IVF cycle. Nevertheless, by selecting genetically normal embryos, PGT can improve IVF success rates, lower the chances of miscarriage, and optimize time-to-pregnancy, making treatment more cost-effective and efficient.

Source: Freepik
Embryo/Egg Cryopreservation
Cryopreservation, the process of freezing eggs or embryos, offers patients the opportunity to preserve their fertility for future use. At Labryo Fertility Center’s IVF lab, we utilize cutting-edge vitrification technology for embryo and egg cryopreservation, ensuring the highest survival and success rates. This advanced flash-freezing technique prevents ice crystal formation, significantly improving post-thaw viability. As such, our lab boasts an exceptional recovery rate of approximately 98% for frozen eggs and embryos.
Some patients may opt for cryopreservation to postpone family planning due to personal or professional plans, preserve fertility before medical treatments, or store extra embryos from an IVF cycle for later use. Studies published in Reproductive Biology and Endocrinology even found that frozen embryo transfers may offer slightly higher pregnancy rates than fresh embryo transfers in certain situations.

Source: Freepik
What Makes Our IVF Lab Exceptional?
Labryo Fertility Center has one of the best IVF labs in the United States. Here’s what makes us stand out:
CAP-Accredited & CLIA-Certified Lab Facility
With a 97.96% fertilization success rate through ICSI and an 86% pregnancy success rate, Labryo Fertility Center’s IVF lab is proudly accredited by the College of American Pathologists (CAP) and certified under the Clinical Laboratory Improvement Amendments (CLIA) as we stay updated with the latest lab protocols. These certifications guarantee that we provide high clinical testing standards, precision in diagnostic procedures, and excellent quality for in-lab IVF procedures, from fertilization to embryo culture and genetic testing.

Quad A-Accredited Procedure Suite
Labryo Fertility Center’s Procedure Suite is fully accredited by the American Association for Accreditation of Ambulatory Surgery Facilities (Quad A). This means we meet 100% of its rigorous standards for patient care, safety protocols, operational efficiency, personnel professionalism, and medical outcomes. In turn, all our patients can have peace of mind knowing we have this prestigious certification that reflects our unwavering commitment to their safety and comfort.

Highly Qualified Team
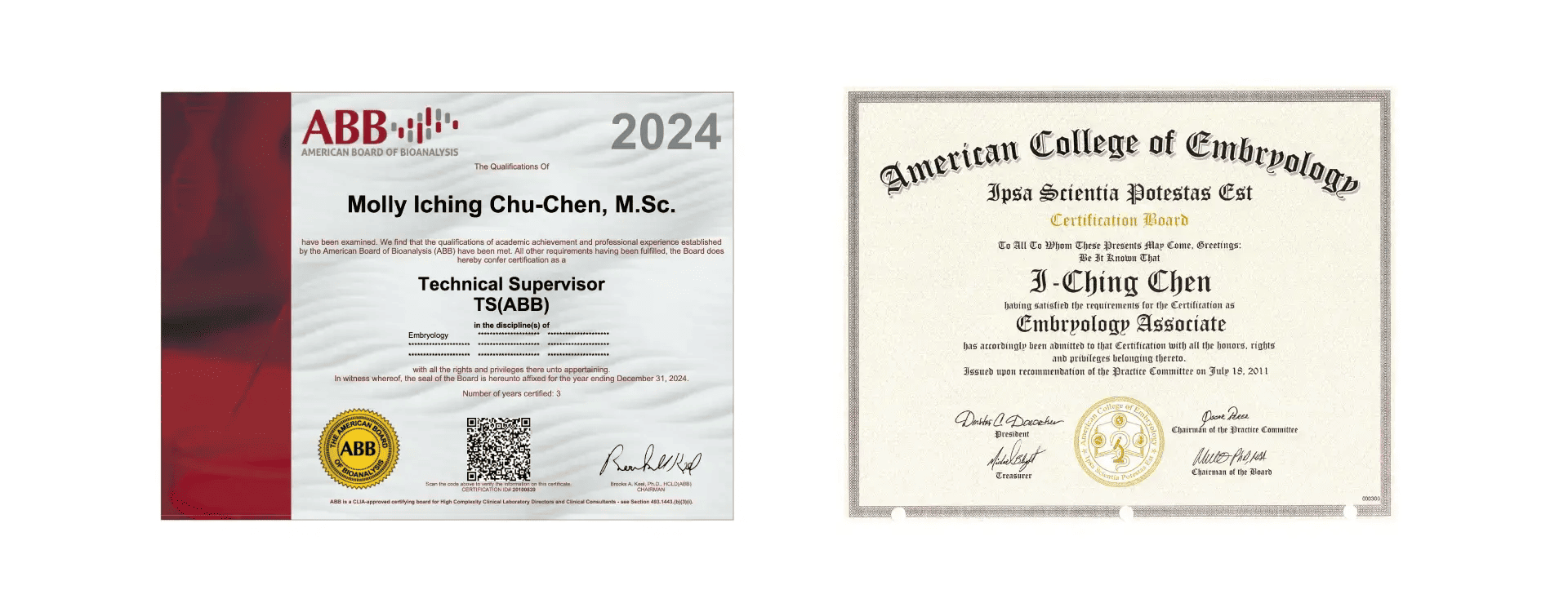
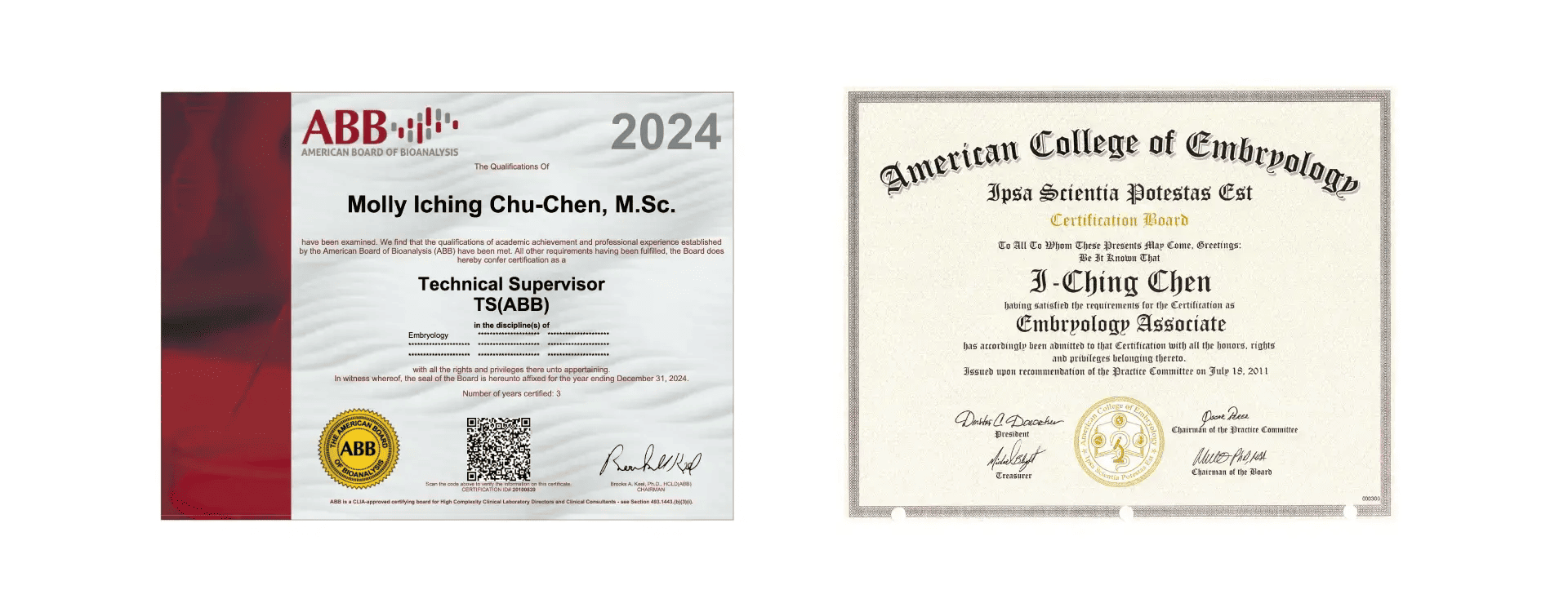
At Labryo Fertility Center, we take pride in our team of highly skilled physicians, embryologists, anesthesiologists, nurses, and clinical staff who hold decades of combined experience and industry-leading credentials, including the ABB (American Board of Bioanalysis) and the American College of Embryology certifications. From pre-operative preparation to post-procedure recovery, this dedicated team ensures a safe and smooth experience for every patient.
Strict Air & Environment Control
The environment within our IVF lab is meticulously controlled to ensure the optimal conditions for embryo development. Embryos are highly sensitive to airborne contaminants such as volatile organic compounds (VOCs), microbes, and dust particles, which can negatively impact their development.
To combat this, we equip the IVF laboratory with HEPA (High-Efficiency Particulate Air) filters, which remove 99.9% of microscopic particles, along with activated carbon filters to eliminate toxic substances.
Furthermore, our dedicated HVAC (Heating, Ventilation, and Air Conditioning) system in the lab and procedure room maintains a stable temperature and humidity level, preventing fluctuations that could stress embryos.
Our lab also serves as a clean environment, with sealed walls, airtight doors, and controlled air pressure to prevent contaminants from entering. With these strict environmental controls, Labryo Fertility Center offers patients the best chance at a healthy pregnancy.
State-of-the-Art Medical Equipment
Our lab houses advanced research-grade tools designed to enhance precision, safety, and efficiency at every stage of the IVF process.

AI Timelapse Incubator (EmbryoScope+)
The EmbryoScope+ incubator features a built-in microscope and camera, capturing images of embryos every 10 minutes to create a time-lapse video. This non-invasive monitoring allows embryologists to select the best embryos for transfer and freezing without removing them from their optimal environment, increasing pregnancy success rates.

Dissecting Microscope
A 100x magnifier that enables embryologists to examine and assess external specimen features, ensuring accurate laboratory results.

Semen Analysis Binocular Microscope
It provides superior image clarity, allowing embryologists to identify and select the best-quality sperm for fertilization.

Spindle View Microscope
This helps assess egg quality at a microscopic level, improving fertilization rates and embryo viability.

Tri-Gas Dry Heat Sterilization Incubator with IR Sensor
This advanced incubator ensures a stable environment for embryo development with HEPA filtration, automatic sensor calibration, and an external sample port to prevent disruptions.
Start Your IVF Journey with Labryo Fertility Center
Whether you're just beginning to explore fertility treatments or looking for more detailed information about our IVF lab, Labryo Fertility Center’s expert team is here to guide you through every step of the process.
Contact us today to schedule a consultation and learn how our state-of-the-art IVF lab and personalized treatment plans can support your dream of parenthood.
Frequently Asked Questions About IVF Labs
Q1. What is an IVF lab?
An IVF lab, also known as an embryology lab, is a specialized facility designed for the delicate handling of eggs, sperm, and embryos. Within this lab, embryologists perform the essential procedures that make IVF possible, from fertilization to embryo culture and selection, all with the goal of increasing the chances of a successful pregnancy.
Q2. How do IVF labs help ensure successful fertilization?
IVF labs maintain precise environmental conditions, including controlled temperature, humidity, and air quality, to support embryo development. It is also important for IVF labs to create a customized lab structure according to the medical staff’s workflow to ensure efficiency for every procedure.
These strict protocols, combined with cutting-edge equipment for continuous monitoring, as well as the skills of experienced embryologists and lab specialists, help optimize fertilization rates and improve the chances of a successful IVF treatment.
Q3. Don’t all fertility clinics have IVF labs?
Not all fertility clinics have an in-house IVF lab. Some clinics partner with external labs, meaning eggs, sperm, and embryos are transported between facilities as the laboratory procedures are outsourced.
It is often best to choose clinics with an on-site IVF lab. This offers significant advantages, including personalized care, streamlined communication, and faster decision-making between doctors and embryologists. This reduces the risk of errors or delays during fertilization, embryo culture, and genetic testing while ensuring stable conditions for these procedures.
The Experts Leading Our IVF Lab Services

Molly Chu-Chen, M.S., M.H.A., TS (ABB)
As the founder and Chief Embryologist at Labryo Fertility Center, Molly Chu-Chen has built an IVF lab where science and compassion come hand-in-hand. She ensures every embryo is cultured under optimal conditions using advanced medical systems. Her background spans prestigious hospitals in the U.S. and Asia, and she remains actively involved in every step—from egg retrieval to embryo transfer—to uphold Labryo Fertility Center’s uncompromising lab standards as they help realize their patients’ dreams of parenthood.
- Technical Supervisor (TS) Certification, American Board of Bioanalysis (ABB)
- M.S. in Clinical Reproductive Science
- M.H.A. in Healthcare Administration
- Embryologist since 1999
- Extensive training and work experience in Taiwan, Singapore, and the United States
Dr. Jeremy A. King, M.D.
Labryo Fertility Center’s cutting-edge IVF lab wouldn’t function without the clinical leadership of Dr. Jeremy King. As Director of IVF, he works closely with embryologists and lab staff to integrate the latest technologies and research into daily practice. His leadership experience in both academic and military settings also ensures that Labryo Fertility Center delivers high-quality, efficient, and personalized fertility care.
- M.D., Saint Louis University School of Medicine
- Residency in Obstetrics and Gynecology, David Grant Medical Center
- Fellowship in Reproductive Endocrinology and Infertility, Johns Hopkins University
- Board Certified in Obstetrics and Gynecology
- Board Certified in Reproductive Endocrinology
- Former Director of the U.S. military’s largest IVF program
- Member, Society of Assisted Reproductive Technology (SART) Registry Committee
