Services
IVF
IVF
What is in vitro fertilization (IVF)?
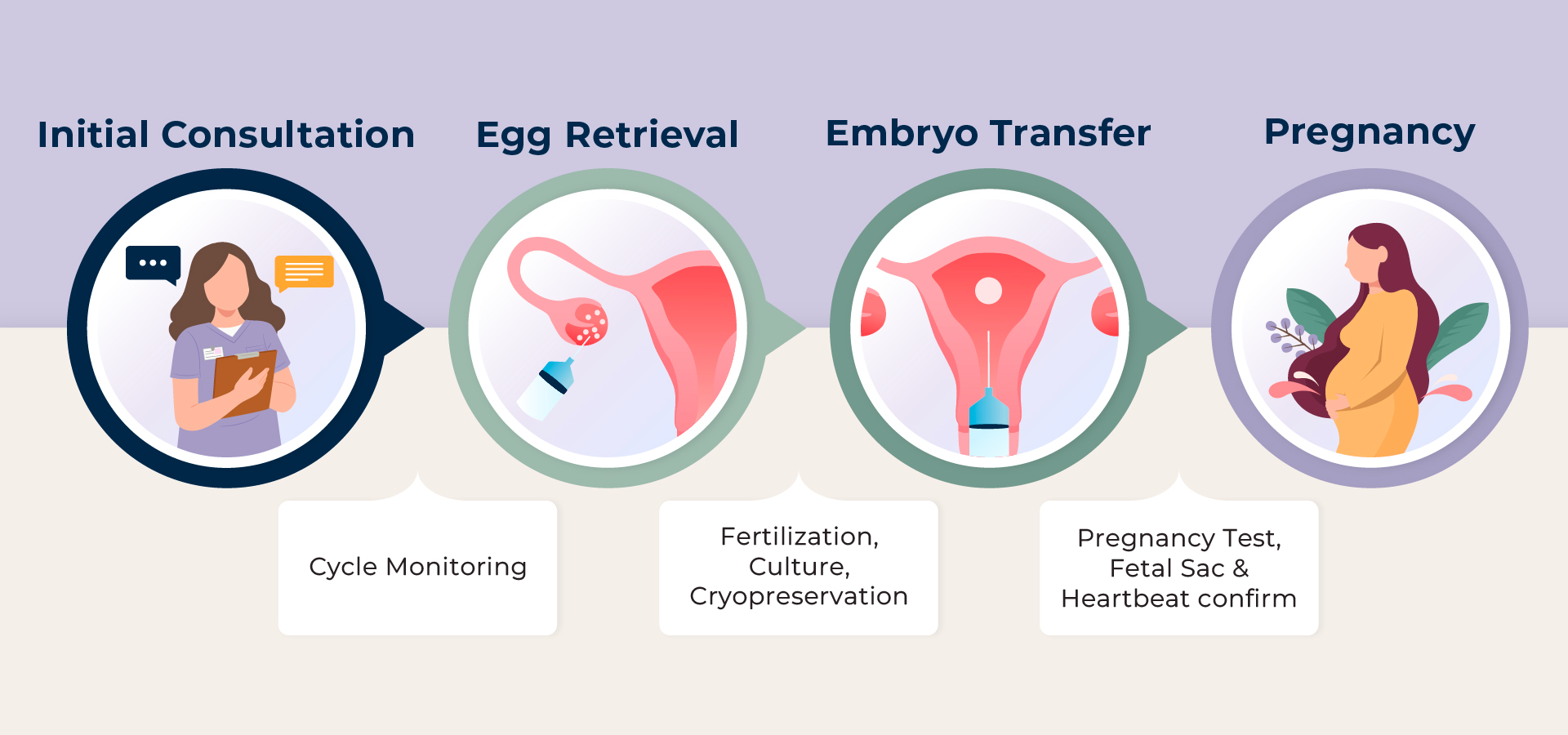
IVF is a method of assisted reproductive technology (ART) in which the sperm and egg are combined outside of the patient’s uterus in a laboratory dish. One or more fertilized eggs (embryos) are then transferred into the woman’s uterus, where the embryo can implant in the uterine lining and begin to develop. Patients can also concurrently cryopreserve (freeze) their extra embryos for future use.
Initially, IVF was introduced to treat women with blocked, damaged, or absent Fallopian tubes. However, today, IVF is used to treat many causes of infertility, such as endometriosis, male factor infertility, PCOS, or unexplained infertility. The basic steps in an IVF treatment cycle are ovarian stimulation, egg retrieval, fertilization, embryo culture, and embryo transfer.

A. Before You Start
These are the steps to proceed with before starting your IVF treatments to ensure you are healthy, prepared, and suitable for IVF.
1. Initial Consultation
Patients are required to have an Initial Consultation with one of our doctors to ensure they meet all Pre-IVF Requirements. Our physician will review your medical history, including any old IVF records, and discuss which treatment options are for you. For out-of-state or international patients, we also offer an initial video consultation.
2. Financial Consultation
One of our financial advisors will meet with patients in person or on the phone to explain our different treatment packages and prices. They will review the fees involved, discuss the various options for each patient, and provide a quote for recommended treatment. At the end of the consultation, the patient needs to sign their quote with a financial agreement before starting the treatment.
3. Consent
It is very important for patients and their partners to read through the consent forms and initial/sign as needed. If the patient doesn’t understand a specific section, please feel free to ask one of our doctors or staff members. If the patient has not signed the given consent form before the appointment, we will be forced to reschedule the appointment. If the consent forms still aren’t signed on the day of the procedure, the procedure may be canceled.
4. Infectious Disease Panel
To be compliant with the regulations of the state law, we are required to conduct infectious disease testing for both you and your partner before every IVF treatment. Patients are required to do a blood test for HIV/AIDS, Hepatitis B & C, Syphilis, Chlamydia, Gonorrhea, and HTLV (male only). HIV/AIDS and Hepatitis B & C are blood-borne infectious diseases that can be transmitted through the placenta and cause long-term health consequences for both the mother and the child. HTLV I & II are human RNA retrovirus that can cause a serious sexually transmitted disease that is related to leukemia, myelopathy, and Syphilis. Infectious disease testing is a necessary preparation before any IVF treatment is started.
5. Pre-IVF Bloodwork
Our physicians may require you to do bloodwork and exams to further evaluate your health and well-being before you begin treatment, such as testing your TSH, Blood Typing, and Pap Smear. Additionally, the physician may have you check for Rubella (German measles) and varicella (chicken pox), which can cause serious birth defects if contracted during pregnancy. These tests help to ensure you are healthy to proceed and have a safe pregnancy.
6. Ovarian Reserve Testing
This test must be done on cycle Day 2 or 3 of your menstrual cycle to evaluate ovarian function. To determine your ovarian reserve, there are several tests available. It is important to know your ovarian reserve before beginning your fertility treatment because it allows us to create a personalized treatment that will show optimal results.
The tests we are currently using in our office are:
- Cycle Day 2 or Cycle Day 3 FSH level (normal range: 5-10mIU/ml)
- Baseline antral follicle counts (AFC) (normal range: 5-10 each ovary)
- AMH (anti-Müllerian hormone) level (normal range: above 2.0ng /ml - this is age dependent)
7. Genetic Testing
The following genetic carrier testing is recommended by the American Society for Reproductive Medicine.
- Cystic fibrosis testing
- Fragile X testing
- Some other genetic testing may be recommended by our doctor after the initial consultation, such as Karyotype and Y chromosome micro-deletion.
8. Pelvic Ultrasound & Saline Infusion Sonogram (SIS) Testing
All patients need a pelvic ultrasound and a SIS test to evaluate the status of the ovaries, tubes, and uterus. The ultrasound can help us evaluate the ovaries and see the uterine size and when any abnormality exists. It can also identify if any fluid has accumulated in the tubes.
A SIS will help to evaluate the uterine cavity and to determine the tubal patency; therefore, it is very important to finish the SIS test before the embryo transfer. Hysterosalpingogram (HSG) and Hysteroscopy are the alternative SIS tests.
B. Treatment Schedule
This is usually the treatment cycle of IVF. Now, there are different ways Labryo can approach the egg retrieval part and the embryo transfer part of IVF, depending on your needs and priority.
Different Approaches to the Egg Retrieval Cycle
1. Stress-Free IVF
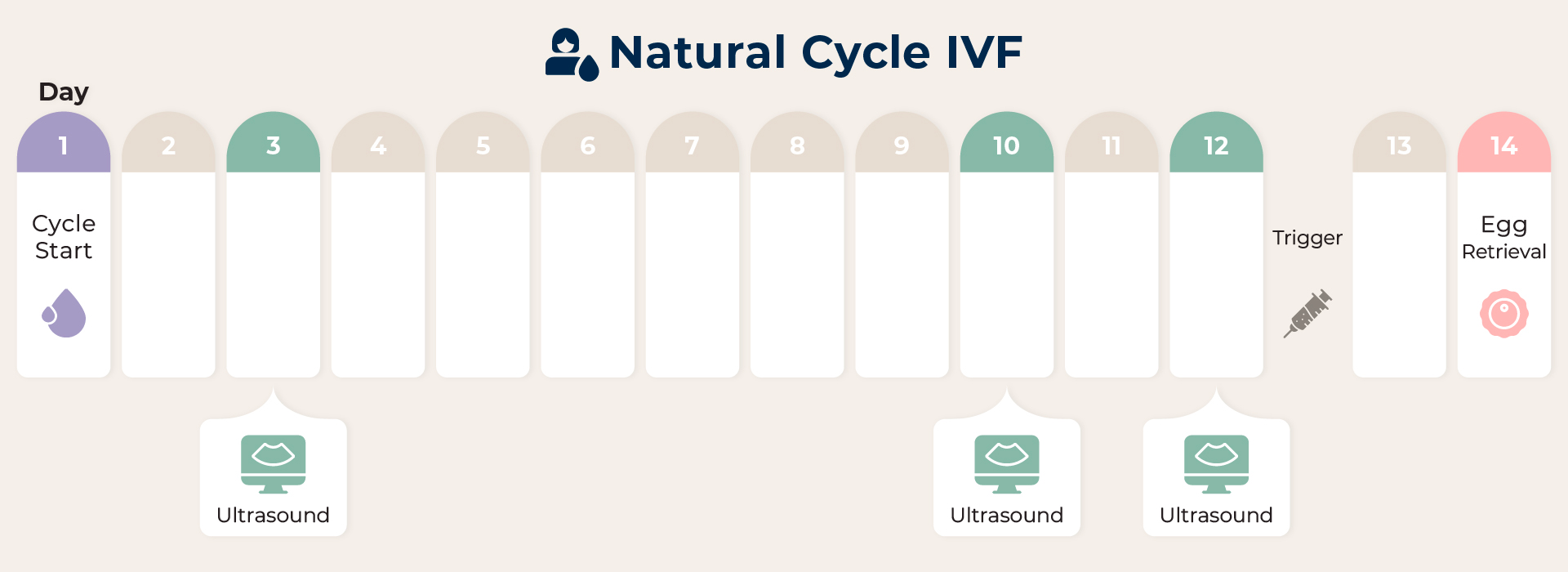
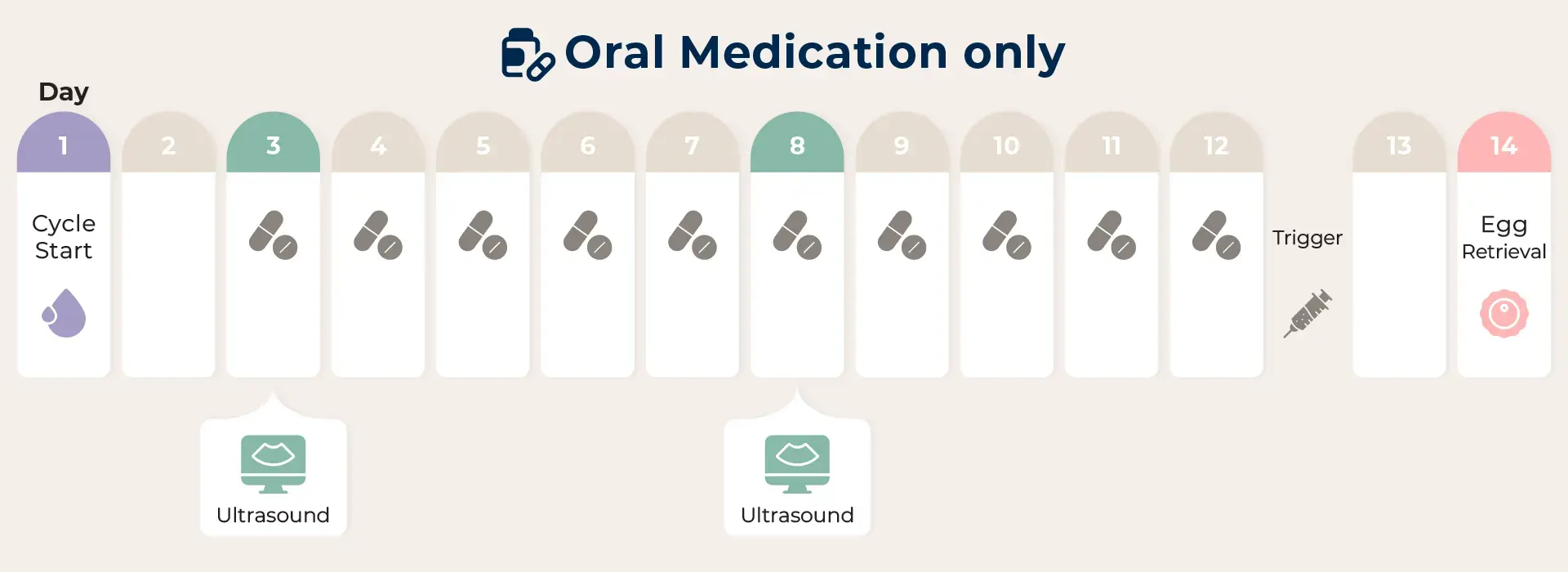
This method is most effective on younger patients or those with a normal menstrual cycle and no problems with ovarian function. With no hormone stimulation or only the use of oral medication to induce follicle maturation, patients have a higher chance of obtaining higher-quality eggs with a low drug impact but will expect to obtain between 1 and 3 eggs per cycle.
2. Mild-Boost IVF
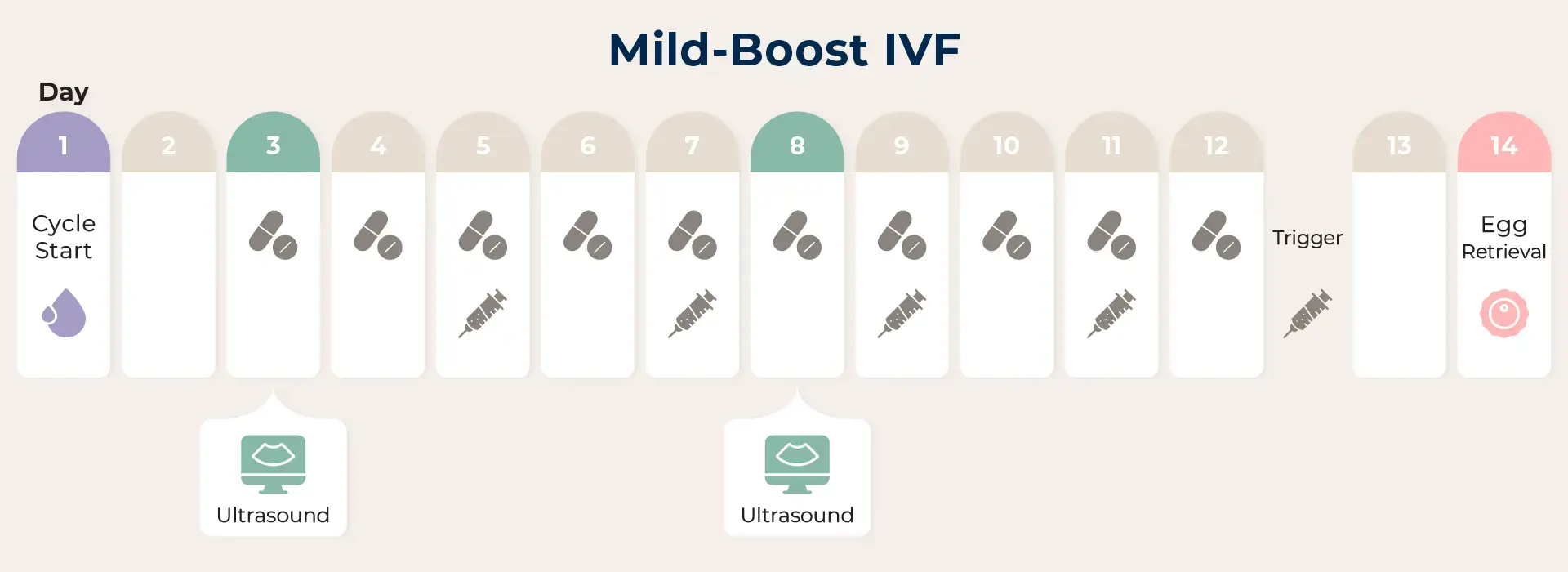
With this treatment, you can expect to attain 5-8 eggs per cycle according to your ovarian function reflected upon the AMH level. In addition to oral medication, minimum doses of hormone injection will be added to your treatment.
3. Classic IVF
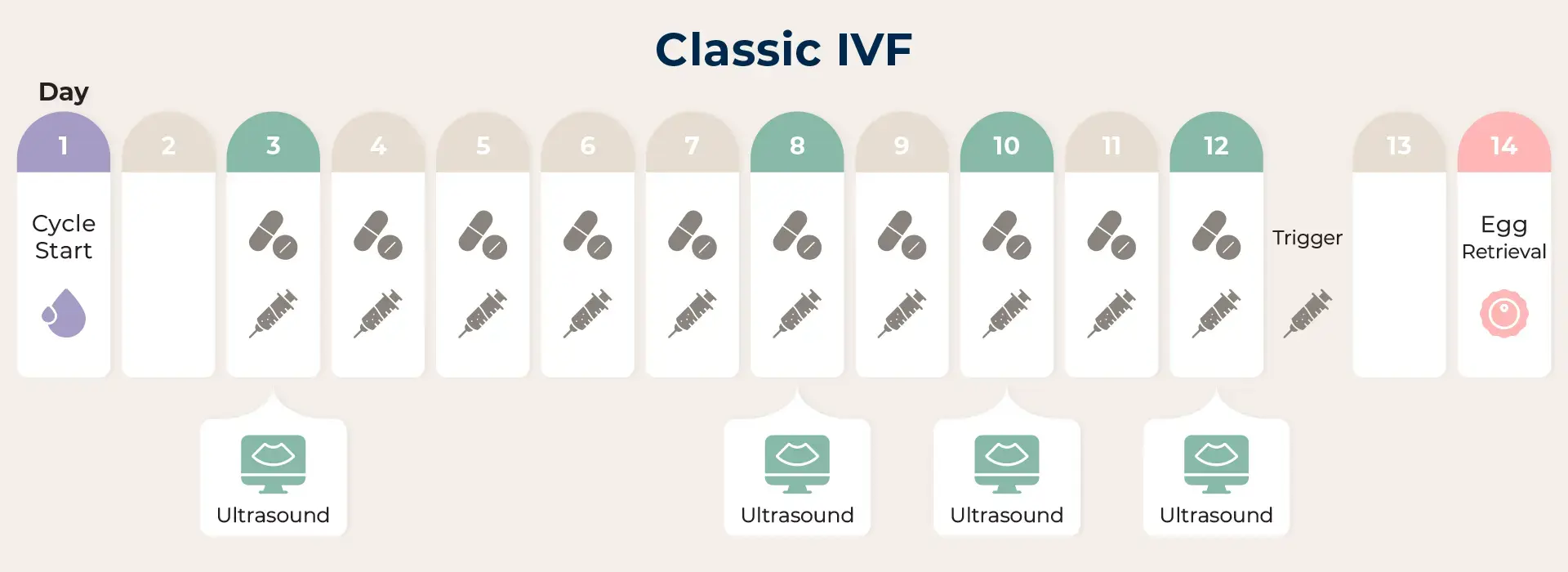
With this treatment protocol, you can expect to attain 5-8 eggs per cycle, depending on your ovarian function, which is influenced by the AMH level. In addition to oral medication, minimum doses of hormone injection will be added to your treatment.
Transvaginal Ooycte Retrieval
The final goal for all of these treatment approaches is to have a successful egg retrieval for the patient. Most patients will be sedated during this procedure, where during this procedure, the physician will aspirate the eggs from the follicles in the ovary while the embryologist will stand by to confirm how many were retrieved. Once all the follicles have been aspirated, the patient will be taken back to the recovery room and can resume regular activity as soon as the following day!
Steps to the Embryo Transfer Cycle
1. Embryo Transfer
The next step in the IVF process is the embryo transfer. This step requires no anesthesia, though some patients may wish to have a mild sedative. In this step, the physician identifies the cervix using a vaginal speculum. One or more embryos that are suspended in a drop of culture medium are drawn into a transfer catheter. The physician then gently guides the tip of the transfer catheter through the cervix and places the fluid containing the embryos into the uterine cavity. This procedure is usually painless, though some women experience mild cramping.
2. Pregnancy Screening
After the embryo transfer, the first pregnancy test will be 10-12 days after the transfer date. It is confirmed with the beta-hCG hormone test. If the pregnancy test is positive, patients will be given further instructions regarding medications and future appointments. The fetus is confirmed by an ultrasound around five weeks of pregnancy, and the fetal heartbeat is confirmed at seven weeks.
After 8-10 weeks of gestation, patients are finished with our clinic’s services and will be referred to a local OB doctor or prenatal specialist for OB care.